Views of a naturalist professional human primate social groomer and neuromatrician
Tuesday, April 24, 2012
Treatment continuum III
9. Locus of control:
On the left side of the diagram, when peoples' bodies develop a frank disease or trauma, operators step in, save life, save limb, or at least try to. The operator assumes the locus of control.
On the right side of the diagram, when people develop non-life threatening conditions, or are recovering from them, or strive to prevent ill health in the first place, helpers interact with people to assist their learning. People retain their own locus of control; the helpers are viewed more as consultants or advisors.
10: The underlying perspective:
On the left, a Cartesian perspective is assumed; namely, body is viewed as something completely separable from the "mind". A third party can intervene, ignore the "mind", deal with the "body", then drop back, and magically the patient's mind and body will return to seamless continuity. This is true, certainly, if loss of consciousness is present.
On the right, a patient's conscious mind/cognizing function is assumed to be intact at all times and part of the entire process. Nothing can happen, really, without the involvement and cooperation of the fully awake and cognizing person receiving the help from the helper. The basic perspective adopted is known as biopsychosocial. No loss of consciousness is involved. In fact, everything hinges on the recipient's attention span, ability to focus, learn, and change his or her own behaviour.
11. Types of operator interventions:
Here we can see types of interventions that could be seen as true operator interventions, i.e., the list with "medical" at the top. In this list, most of the procedures require some sort of anesthesia.
The second list is in the operator side of the picture because the "operators" performing the function have learned to do their work (inappropriately) from a bottom up Cartesian perspective. There is no anesthesia required or dispensed. These approaches could be characterized as coercive, although the operators have the option of learning how to perform them in a more interactive fashion.
The "operators" in this list imagine
1. that they have locus of control,
2. that they are affecting the patient from the outside, the body, in.
In my opinion, they are deluding themselves, and their patients, simply by the way they were taught to think (inadvertently), or else deliberately. In any case, they (mostly) do not consider the nervous system in their reasoning, nor do they imagine their treatment to have any direct effect on it, or that it might produce different output based on novel input; rather they tend to assume that the work they do on their tissue of choice eventually has been registered positively by the patient's passive nervous system. They allow themselves to imagine they have accomplished something outside the organism's control, and take full credit for getting the job done right.
12. Types of interactor interventions:
This includes anything anyone does to anyone which involves acknowledgement of the awareness and conscious veto power of the human nervous system, from its most peripheral, to its innermost central aspects. It includes a broad spectrum from the most committed one-to-one physical contact, to hands-off group work, to social programs designed to benefit the entire troop from top to bottom and over time.
To the left we see massage, right at the border between mesoderm and ectoderm, focusing on "muscle" but also on treatment dyad dynamics.
Beside it we see neurodynamics. This is a recently evolved treatment method whereby nerves are slid about through limbs and spines. It evolved out of "ortho", still retains a focus on "tissue", but the main focus is now on pain as an output, so it has moved further to the right, into the domain of ectodermal, of biopsychosocial.
Just to the right of that, we see DNM. This is my baby. It stands for dermoneuromodulation. It also evolved toward the right, and away from operator methods and massage. Focus is on cutaneous nerves, pain as a biopsychosocial brain output. It assumes that non-nociceptive novel input will result in altered (usually less) pain output.
To the right of it, we see SC. SC stands for simple contact, Barrett Dorko's baby. It deals with the peripheral nerves and nervous system as well, but leans a bit more toward different movement output based on novel input.
Beside its right, we see a whole host of exercise schools of thought. Exercise can do wonders for practically anything.
Moving further to the right, we have several examples of purely interactive strategies at group, societal and individual levels.
13. Putting it all together:
Here is the whole thing, finally. It's a busy slide, may need tinkering, but most of it is accounted for I think.
TREATMENT CONTINUUM I
TREATMENT CONTINUUM II
Treatment continuum II
6. Pattern recognition and explanation:
PATTERNICITY, ABSTRACTION, CONCEPTUALIZATION, APOPHENIA:
Because we are human, we do mental activity known as abstraction and conceptualization. We can't help ourselves. Things just turned out that way. Our brains evolved to recognize patterns, even false ones, and build conceptual baskets in which to store them, and from where we can retrieve them later, or compare them to new patterns we see in the moment. It also evolved to believe that conceptualizations and abstractions, symbols for real things, are just as real as the things they symbolize.
The brain is a zoom lens. It distorts everything, including knowledge. So, science developed in order to correct for that. It's a way of smoothing out distortion of individuals by comparing more knowledge and more conceptual baskets than a single human brain ever could, using mathematical and statistical tools that have been agreed, collectively, do the job, if not to complete perfection, at least a whole lot more objectively than just one person's opinion. This clears away a lot of conceptual clutter.
EVIDENCE-BASED:
"Evidence-based" means that someone scientifically quantified the results from a bunch of interventions, and was able to show there was a "statistically significant" result, a positive treatment effect, that lasted over a given period of time. If it did this in the past, it is likely to be able to do this into the future, over time, become "predictable" which increases confidence in the method.
MECHANISM:
Evidence-based does not explain mechanism however. Other kinds of science (also relying on quantifiability) delve into mechanism and ultimately, converge to produce the world of thought's Best Guess as to What Might be Going on.
7. That which lies outside scientific scrutiny:
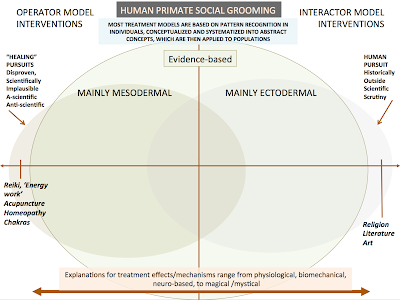
Here we see arrows on each side pointing to what is outside the range of evidence-based treatment.
In my mind (with all its individual bias) I see what is to the left, as being body-targeted interventions or conceptualizations, based on premises which have been disproven over time.
On the right, the bulge sticking outside the border of science represents human pursuits mostly uninteresting to or inaccessible by science (although science has made inroads there anyway).
8. Below are what, in my own mind, belong in these two groups of items.
This leaves us with that big empty area in the middle to fill up. Which is where we are going next.
TREATMENT CONTINUUM I
TREATMENT CONTINUUM III
PATTERNICITY, ABSTRACTION, CONCEPTUALIZATION, APOPHENIA:
Because we are human, we do mental activity known as abstraction and conceptualization. We can't help ourselves. Things just turned out that way. Our brains evolved to recognize patterns, even false ones, and build conceptual baskets in which to store them, and from where we can retrieve them later, or compare them to new patterns we see in the moment. It also evolved to believe that conceptualizations and abstractions, symbols for real things, are just as real as the things they symbolize.
The brain is a zoom lens. It distorts everything, including knowledge. So, science developed in order to correct for that. It's a way of smoothing out distortion of individuals by comparing more knowledge and more conceptual baskets than a single human brain ever could, using mathematical and statistical tools that have been agreed, collectively, do the job, if not to complete perfection, at least a whole lot more objectively than just one person's opinion. This clears away a lot of conceptual clutter.
EVIDENCE-BASED:
"Evidence-based" means that someone scientifically quantified the results from a bunch of interventions, and was able to show there was a "statistically significant" result, a positive treatment effect, that lasted over a given period of time. If it did this in the past, it is likely to be able to do this into the future, over time, become "predictable" which increases confidence in the method.
MECHANISM:
Evidence-based does not explain mechanism however. Other kinds of science (also relying on quantifiability) delve into mechanism and ultimately, converge to produce the world of thought's Best Guess as to What Might be Going on.
7. That which lies outside scientific scrutiny:
Here we see arrows on each side pointing to what is outside the range of evidence-based treatment.
In my mind (with all its individual bias) I see what is to the left, as being body-targeted interventions or conceptualizations, based on premises which have been disproven over time.
On the right, the bulge sticking outside the border of science represents human pursuits mostly uninteresting to or inaccessible by science (although science has made inroads there anyway).
8. Below are what, in my own mind, belong in these two groups of items.
This leaves us with that big empty area in the middle to fill up. Which is where we are going next.
TREATMENT CONTINUUM I
TREATMENT CONTINUUM III
Treatment continuum I
Rather than write write write to describe how I view the treatment spectrum, I have made a bunch of pictures illustrating how I have come to view the archeology of it over time.
1. We start with a simple diagram of a human organism:
Every human organism starts out as a single cell, which becomes a two-layered blob, ectoderm on top and endoderm on the bottom. Ectoderm builds the nervous system.
Ectoderm gives off some cells which leak down under it, between the two layers, called mesoderm.
2. Mesoderm builds the structural parts of the body.
3. When we put them together we get this:
The peripheral nervous system is where the two overlap.
So, very simple, very schematically, this is what we treat.
The patient is alive, conscious, his or her brain straining to understand what it must do to cooperate.
We provide said brain with some good pain education, before we "do" anything else.
4. Here is a simple diagram to represent all interventions anyone makes for anyone. It's expandable.
5. When laid over top of the human organism we end up with something like this:
The larger circle in front represents that which can be scientifically studied, and evidence obtained.
OPERATOR MODELS:
"Operator model interventions", on the left, target the "body". These are generally "practitioner knows best" types of interventions. The patient may be informed but the treatment plan is well-worn and not particularly subject to debate.
INTERACTOR MODELS:
On the right, we see "Interactor model interventions" which include the patient him or herself, the patient's conscious awareness, seek to obtain permission and cooperation, active participation. The patient is taught that they retain full locus of control, and how to use it. They are encouraged to provide feedback and think of possible alterations to the plan themselves. Together the practitioner and the patient map out a path together, over time.
For more about these two ways of thinking about treating patients, see this google document on the topic.
The line of demarcation between the two isn't usually as clear as it appears in the picture.
More to come.
TREATMENT CONTINUUM II
TREATMENT CONTINUUM III
Operator/Interactor models (google doc)
1. We start with a simple diagram of a human organism:
Every human organism starts out as a single cell, which becomes a two-layered blob, ectoderm on top and endoderm on the bottom. Ectoderm builds the nervous system.
Ectoderm gives off some cells which leak down under it, between the two layers, called mesoderm.
2. Mesoderm builds the structural parts of the body.
3. When we put them together we get this:
The peripheral nervous system is where the two overlap.
So, very simple, very schematically, this is what we treat.
The patient is alive, conscious, his or her brain straining to understand what it must do to cooperate.
We provide said brain with some good pain education, before we "do" anything else.
4. Here is a simple diagram to represent all interventions anyone makes for anyone. It's expandable.
5. When laid over top of the human organism we end up with something like this:
The larger circle in front represents that which can be scientifically studied, and evidence obtained.
OPERATOR MODELS:
"Operator model interventions", on the left, target the "body". These are generally "practitioner knows best" types of interventions. The patient may be informed but the treatment plan is well-worn and not particularly subject to debate.
INTERACTOR MODELS:
On the right, we see "Interactor model interventions" which include the patient him or herself, the patient's conscious awareness, seek to obtain permission and cooperation, active participation. The patient is taught that they retain full locus of control, and how to use it. They are encouraged to provide feedback and think of possible alterations to the plan themselves. Together the practitioner and the patient map out a path together, over time.
For more about these two ways of thinking about treating patients, see this google document on the topic.
The line of demarcation between the two isn't usually as clear as it appears in the picture.
More to come.
TREATMENT CONTINUUM II
TREATMENT CONTINUUM III
Operator/Interactor models (google doc)
Saturday, April 07, 2012
Pain and tissue damage are from different planets.
Kory Zimney at SomaSimple found and collected together a bunch of papers showing the complete lack of predictable correlation between "tissue damage" and pain, in the neck, shoulder and low back. Many of them are open access, so I thought I'd collect them here, too.
1. Magnetic Resonance Imaging of the Lumbar Spine in People Without Back Pain.
2. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation
(You mean, like a third ... of ordinary people walking around without any pain, have a verifiably trashed back?)
3. MRI Findings in Throwing Shoulders
(Structural abnormalities don't go together with shoulder pain in pitchers? What? No correlation between tissue "damage" and pain?)
4. MRI of cervical intervertebral discs in asymptomatic subjects
(Even spinal cord compression? No symptoms? Wow. See? Asymptomatic people, bad images, pain and tissue damage have nothing to DO with each other!)
5. Natural history of lumbar disc hernia with radicular leg pain: Spontaneous MRI changes of the herniated mass and correlation with clinical outcome
(Seriously? These things go away all by themselves? What?? Get out of town!)
1. Magnetic Resonance Imaging of the Lumbar Spine in People Without Back Pain.
AbstractBACKGROUND:The relation between abnormalities in the lumbar spine and low back pain is controversial. We examined the prevalence of abnormal findings on magnetic resonance imaging (MRI) scans of the lumbar spine in people without back pain.METHODS:We performed MRI examinations on 98 asymptomatic people. The scans were read independently by two neuroradiologists who did not know the clinical status of the subjects. To reduce the possibility of bias in interpreting the studies, abnormal MRI scans from 27 people with back pain were mixed randomly with the scans from the asymptomatic people. We used the following standardized terms to classify the five intervertebral disks in the lumbosacral spine: normal, bulge (circumferential symmetric extension of the disk beyond the interspace), protrusion (focal or asymmetric extension of the disk beyond the interspace), and extrusion (more extreme extension of the disk beyond the interspace). Nonintervertebral disk abnormalities, such as facet arthropathy, were also documented.RESULTS:Thirty-six percent of the 98 asymptomatic subjects had normal disks at all levels. With the results of the two readings averaged, 52 percent of the subjects had a bulge at at least one level, 27 percent had a protrusion, and 1 percent had an extrusion. Thirty-eight percent had an abnormality of more than one intervertebral disk. The prevalence of bulges, but not of protrusions, increased with age. The most common nonintervertebral disk abnormalities were Schmorl's nodes (herniation of the disk into the vertebral-body end plate), found in 19 percent of the subjects; annular defects (disruption of the outer fibrous ring of the disk), in 14 percent; and facet arthropathy (degenerative disease of the posterior articular processes of the vertebrae), in 8 percent. The findings were similar in men and women.CONCLUSIONS:On MRI examination of the lumbar spine, many people without back pain have disk bulges or protrusions but not extrusions. Given the high prevalence of these findings and of back pain, the discovery by MRI of bulges or protrusions in people with low back pain may frequently be coincidental.(What?? Over HALF of all these asymptomatic, no pain, no complaints, people, have a disc bulge??)
2. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation
We performed magnetic resonance imaging on sixty-seven individuals who had never had low-back pain, sciatica, or neurogenic claudication. The scans were interpreted independently by three neuro-radiologists who had no knowledge about the presence or absence of clinical symptoms in the subjects. About one-third of the subjects were found to have a substantial abnormality. Of those who were less than sixty years old, 20 per cent had a herniated nucleus pulposus and one had spinal stenosis. In the group that was sixty years old or older, the findings were abnormal on about 57 per cent of the scans: 36 per cent of the subjects had a herniated nucleus pulposus and 21 per cent had spinal stenosis. There was degeneration or bulging of a disc at at least one lumbar level in 35 per cent of the subjects between twenty and thirty-nine years old and in all but one of the sixty to eighty-year-old subjects. In view of these findings in asymptomatic subjects, we concluded that abnormalities on magnetic resonance images must be strictly correlated with age and any clinical signs and symptoms before operative treatment is contemplated.
(You mean, like a third ... of ordinary people walking around without any pain, have a verifiably trashed back?)
3. MRI Findings in Throwing Shoulders
Shoulders of throwing athletes are highly stressed joints and likely to have more structural abnormalities seen on magnetic resonance imaging scans. Prevalence and type of structural abnormalities, especially abnormalities of the rotator cuff tendons and the superolateral humeral head, and correlation of magnetic resonance imaging findings with symptoms and clinical tests, are not well known. Throwing and nonthrowing (symptomatic and asymptomatic) shoulders of 30 fully competitive professional handball players and 20 dominant shoulders of randomly selected volunteers were evaluated for comparison clinically and with magnetic resonance imaging. An average of seven abnormal magnetic resonance imaging findings was observed in the throwing shoulders; more than in the nonthrowing and the control shoulders. Although 93% of the throwing shoulders had abnormal magnetic resonance imaging findings, only 37% were symptomatic. Partial rotator cuff tears and mainly superolateral osteochondral defects of the humeral head were identified as typical throwing lesions. Symptoms correlated poorly with abnormalities seen on magnetic resonance imaging scans and findings from clinical tests. This suggests that the evaluation of an athlete’s throwing shoulder should be done very thoroughly and should not be based mainly on abnormalities seen on magnetic resonance imaging scans.
(Structural abnormalities don't go together with shoulder pain in pitchers? What? No correlation between tissue "damage" and pain?)
4. MRI of cervical intervertebral discs in asymptomatic subjects
We studied degenerative changes in the cervical intervertebral discs of 497 asymptomatic subjects by MRI and evaluated disc degeneration by loss of signal intensity, posterior and anterior disc protrusion, narrowing of the disc space and foraminal stenosis. In each subject, five disc levels from C2-C3 to C6-C7 were evaluated.
The frequency of all degenerative findings increased linearly with age. Disc degeneration was the most common observation, being present in 17% of discs of men and 12% of those of women in their twenties, and 86% and 89% of discs of both men and women over 60 years of age. We found significant differences in frequency between genders for posterior disc protrusion and foraminal stenosis. The former, with demonstrable compression of the spinal cord, was observed in 7.6% of subjects, mostly over 50 years of age.
Our results should be taken into account when interpreting the MRI findings in patients with symptomatic disorders of the cervical spine.
(Even spinal cord compression? No symptoms? Wow. See? Asymptomatic people, bad images, pain and tissue damage have nothing to DO with each other!)
5. Natural history of lumbar disc hernia with radicular leg pain: Spontaneous MRI changes of the herniated mass and correlation with clinical outcome
A prospective sequential MRI study was done to investigate the morphologic changes of the lumbar disc hernia(LDH). We also studied the relationship between the MRI changes and the type of LDH and the clinical outcome. MRI was performed every 3 months from the onset for a maximum of 24 months in 42 patients with radicular leg pain and symptoms definitely diagnosed as caused by LDH. The size of the herniated mass was determined by the ratio of the anteroposterior diameter of the spinal canal to the maximum diameter of the LDH mass on T2-weighted axial images.
The clinical outcome was evaluated as excellent, good, or poor depending on leg pain and physical findings. The JOA (Japanese Orthopaedic Association) score for LDH was also used to assess the outcome.
Thirty-seven (88%) of the 42 patients showed >50% reduction of the hernia on MRI 3–12 months after onset, and the morphologic changes of the herniated mass were well correlated with the clinical outcome.
(Seriously? These things go away all by themselves? What?? Get out of town!)
Thursday, April 05, 2012
At laaaaaaaaast....
"At laaaaaaaast.... my table's come along......"
Sorry Etta James, couldn't resist. The feeling is exactly right. (Minus the kinesthetic display in the video, apart from its symbolic beauty, I mean.)
Yup. Monday at 1:15 PM, the new table is to be delivered unto me.. or at least into the space I've been renting (hopefully, in anticipation) all winter. But not working in, because I did not have this beautiful table I expect with people upon, for the rest of my working days, being 61 and all.
I was in stasis mode. For months. Everything was completely out of my control, and all I could do was hang in there until things sorted themselves out.
Why? What was going on?
I arranged to rent working space, in advance of having adequate equipment, last October. When I had space secured, I ordered a treatment table. It was supposed to take ten weeks to be built in Belgium, imported, then moved to my little city in the prairies.
Well, it took longer than that, and I still don't know the whole story, because the guy in quebec who is the Canadian connection is very contained about all of it. Anyway, it was supposed to be here in January, but is now 2 and a half months overdue.
But today, the local moving company, here in my own town, called to arrange delivery. I learned the table weighs 302 pounds. That's a lot. But what I like is that it's a concrete detail, and concrete details reassure me. That it exists. That it's here. That soon I'll be able to start using it.
The treatment room is in a spa, which is OK, because at least it smells good there.. My practice will have nothing to do with the spa business - it's just a room I'm renting there. I'll be my own business.
In November, December, I got the place furnished, in anticipation, with a name registered in the province, a phone (not yet connected, but with a number that I'm paying for every month), a desk, a partition dividing the space into treatment area and reception area, a file cabinet (a lateral three-drawer affair, which I hope will suffice to contain all the patient files I expect to accumulate for the rest of my life).
A lamp, because (alas!) the place does not have natural light, no window. (Which is if I'm really honest, a good chunk of the reason why I never moved in all winter even though I had procured a massage table - I couldn't bear to start up in a place with no window during the winter.)
So, in some ways, the timing worked out fine. I think I can stand working in there during summer, and I am negotiating with the landlady/spa-owner for a window to be installed, even just a light pipe would be a big help..
It HAS been nice, pretending to be retired - it gave me a great rest for almost 3 years, but the writing's on the wall; I've run out of surplus cash from having sold a paid-off condo in ridiculously expensive Vancouver. I've lost a pile of weight and gained a bunch of muscle. I'm ready to roam the world teaching, and maintain a completely relaxed practice to pay for groceries. Time to get busy I guess. And yes, I feel better. Not great, but better. Probably good enough. Bring it - I'm up for it.
Sorry Etta James, couldn't resist. The feeling is exactly right. (Minus the kinesthetic display in the video, apart from its symbolic beauty, I mean.)
Yup. Monday at 1:15 PM, the new table is to be delivered unto me.. or at least into the space I've been renting (hopefully, in anticipation) all winter. But not working in, because I did not have this beautiful table I expect with people upon, for the rest of my working days, being 61 and all.
I was in stasis mode. For months. Everything was completely out of my control, and all I could do was hang in there until things sorted themselves out.
Why? What was going on?
I arranged to rent working space, in advance of having adequate equipment, last October. When I had space secured, I ordered a treatment table. It was supposed to take ten weeks to be built in Belgium, imported, then moved to my little city in the prairies.
Well, it took longer than that, and I still don't know the whole story, because the guy in quebec who is the Canadian connection is very contained about all of it. Anyway, it was supposed to be here in January, but is now 2 and a half months overdue.
But today, the local moving company, here in my own town, called to arrange delivery. I learned the table weighs 302 pounds. That's a lot. But what I like is that it's a concrete detail, and concrete details reassure me. That it exists. That it's here. That soon I'll be able to start using it.
The treatment room is in a spa, which is OK, because at least it smells good there.. My practice will have nothing to do with the spa business - it's just a room I'm renting there. I'll be my own business.
In November, December, I got the place furnished, in anticipation, with a name registered in the province, a phone (not yet connected, but with a number that I'm paying for every month), a desk, a partition dividing the space into treatment area and reception area, a file cabinet (a lateral three-drawer affair, which I hope will suffice to contain all the patient files I expect to accumulate for the rest of my life).
A lamp, because (alas!) the place does not have natural light, no window. (Which is if I'm really honest, a good chunk of the reason why I never moved in all winter even though I had procured a massage table - I couldn't bear to start up in a place with no window during the winter.)
So, in some ways, the timing worked out fine. I think I can stand working in there during summer, and I am negotiating with the landlady/spa-owner for a window to be installed, even just a light pipe would be a big help..
It HAS been nice, pretending to be retired - it gave me a great rest for almost 3 years, but the writing's on the wall; I've run out of surplus cash from having sold a paid-off condo in ridiculously expensive Vancouver. I've lost a pile of weight and gained a bunch of muscle. I'm ready to roam the world teaching, and maintain a completely relaxed practice to pay for groceries. Time to get busy I guess. And yes, I feel better. Not great, but better. Probably good enough. Bring it - I'm up for it.
Tuesday, April 03, 2012
Ah, now I remember.
I read a little thing this morning about Duchenne Muscular Dystrophy in this blogpost, and immediately recalled an event that happened while doing clinical training in PT school, over 40 years ago. We were still in school, but each morning we had to go to some assigned hospital to work with actual patients.
One of my patients one morning was a young boy, maybe 10 or 11 years old, with DMD. His lungs were full of sputum and he was too weak to cough effectively. His dad was there, sitting beside him. My job was to handle his chest wall to help support him to cough, and breathe. I'd been taught all sorts of fancy positions to supposedly aid in this effort, and got busy.
I really got into my task, and promptly lost track of time. The story of my life. I worked and worked and worked with him, and the kid expelled a great deal of sputum. Success. His dad sat by his side, watching hopefully, remaining contained, a silent and steady support. I was barely out of being a kid myself (18 at the time), and I was glad he was there.
After what seemed like five minutes had passed, but in reality had been almost an hour probably, another PT student came in, looking for me.
This had been my first conscious experience of having immersed myself in free-falling interaction with another person's nervous system, then being rudely brought back to unwelcome social exigency, at the expense of the process that had begun to unfold and which I felt completely part of. I remember that I felt confused and resentful, all mixed together. Sort of the story of my whole life, actually, now that I think about it. There has always been that kind of grind in my gears.
I took another look at the task: the kid was breathing much easier now, and I was fairly pleased with the job I had done. The dad was pleased too, and tried to reward me. He said, "I want you to have this pen." (He had quickly fished around for a present and had found it in his shirt.)
We had just had a big lecture in the department about how it was wrong to accept any gifts or money from patients, to gracefully refuse. So I tried to. It felt awkward and uncomfortable. Here was a guy genuinely trying to compensate me, as part of a completion of a therapeutic ritual which had been (at least temporarily) successful; he was genuinely grateful, and could probably see that I was struggling to unfold into a good therapist, wanted to mark his attendance at this event somehow, so, had been moved to do this, make this gesture. It wasn't just empty gesture. Even I could sense this, and I'm not really great at telling the difference. So, I tried, but in the end, I accepted his gift of his own 29 cent ballpoint pen, as a symbol of his own completion of a psychosocial moment, and expression of his own gratitude. I did not think I had any right to refuse, on that level. I mean, here was a guy watching his own son die slowly - I knew full well I'd never in a million years ever have the strength or grace to do anything like it. I was embarrassed about my robust health and good fortune in life. If he wanted me to have a dumb pen, then he had the right to bestow it, because he had earned that right.
I went to rejoin the human primate social grooming squad I had signed up to travel with through this phase of my life and training, but always kept an eye open for some way not to have to be subject to group dynamics and behaviour if I didn't want to, as it always has seemed mostly annoying and interruptive, as opposed to welcome and distracting. Looking back I can see now that all the discomfort I felt led me out of hospital work and toward working with pure pain in patients, and independently, as a solo practitioner, in order to be able to lose myself in the interactive process with no interruption.
One of my patients one morning was a young boy, maybe 10 or 11 years old, with DMD. His lungs were full of sputum and he was too weak to cough effectively. His dad was there, sitting beside him. My job was to handle his chest wall to help support him to cough, and breathe. I'd been taught all sorts of fancy positions to supposedly aid in this effort, and got busy.
I really got into my task, and promptly lost track of time. The story of my life. I worked and worked and worked with him, and the kid expelled a great deal of sputum. Success. His dad sat by his side, watching hopefully, remaining contained, a silent and steady support. I was barely out of being a kid myself (18 at the time), and I was glad he was there.
After what seemed like five minutes had passed, but in reality had been almost an hour probably, another PT student came in, looking for me.
PT student: "Why didn't you answer your page?"
Me: "What page? You were paging me? Why?"
PT student: "You were supposed to be back in the department by 10 AM so we could all go to coffee together."
Me: "Oh. Gee, sorry, I completely lost track of time, forgot, didn't hear the page. OK, I'll be there in a minute."PT student hurried off in order to enjoy her coffee and hang with the group.
This had been my first conscious experience of having immersed myself in free-falling interaction with another person's nervous system, then being rudely brought back to unwelcome social exigency, at the expense of the process that had begun to unfold and which I felt completely part of. I remember that I felt confused and resentful, all mixed together. Sort of the story of my whole life, actually, now that I think about it. There has always been that kind of grind in my gears.
I took another look at the task: the kid was breathing much easier now, and I was fairly pleased with the job I had done. The dad was pleased too, and tried to reward me. He said, "I want you to have this pen." (He had quickly fished around for a present and had found it in his shirt.)
We had just had a big lecture in the department about how it was wrong to accept any gifts or money from patients, to gracefully refuse. So I tried to. It felt awkward and uncomfortable. Here was a guy genuinely trying to compensate me, as part of a completion of a therapeutic ritual which had been (at least temporarily) successful; he was genuinely grateful, and could probably see that I was struggling to unfold into a good therapist, wanted to mark his attendance at this event somehow, so, had been moved to do this, make this gesture. It wasn't just empty gesture. Even I could sense this, and I'm not really great at telling the difference. So, I tried, but in the end, I accepted his gift of his own 29 cent ballpoint pen, as a symbol of his own completion of a psychosocial moment, and expression of his own gratitude. I did not think I had any right to refuse, on that level. I mean, here was a guy watching his own son die slowly - I knew full well I'd never in a million years ever have the strength or grace to do anything like it. I was embarrassed about my robust health and good fortune in life. If he wanted me to have a dumb pen, then he had the right to bestow it, because he had earned that right.
I went to rejoin the human primate social grooming squad I had signed up to travel with through this phase of my life and training, but always kept an eye open for some way not to have to be subject to group dynamics and behaviour if I didn't want to, as it always has seemed mostly annoying and interruptive, as opposed to welcome and distracting. Looking back I can see now that all the discomfort I felt led me out of hospital work and toward working with pure pain in patients, and independently, as a solo practitioner, in order to be able to lose myself in the interactive process with no interruption.
Subscribe to:
Posts (Atom)